Access to contraception is one of the most effective tools for empowering women and improving global health, yet in 2024, 164 million women of reproductive age still lack the resources they need.
Despite decades of progress, barriers like cost, misinformation, social stigma, and geographical gaps persist, leaving millions—particularly in regions like Sub-Saharan Africa and South Asia—without reliable options.
Why does access remain so uneven, and how does it impact women’s lives?
By exploring the disparities in contraceptive access across countries, we’ll uncover how this issue shapes everything from education to economic stability and how, by closing these gaps, we can move closer to true gender equality worldwide.
Key Milestones
- 1960: Introduction of the contraceptive pill in the United States, Germany, and other countries.
- 1979: The Convention on the Elimination of All Forms of Discrimination Against Women (CEDAW) established a mandate for women’s right to family planning education and services.
- 1994: The International Conference on Population and Development emphasized reproductive health as a critical global priority.
- 2007: The establishment of World Contraception Day to raise awareness of the importance of family planning.
These milestones have shaped policies and programs worldwide, but challenges persist, especially in low- and middle-income countries.
Why Contraceptive Access Matters

Contraceptive access isn’t just a personal health issue; it’s a global health and economic issue with direct ties to gender equality.
The United Nations’ Sustainable Development Goals (SDGs), specifically SDG 3 (Good Health and Well-being) and SDG 5 (Gender Equality), aim to ensure universal access to reproductive health care, including contraception.
Having access to contraception gives women the freedom to plan their families, pursue education and work opportunities, and reduce health risks associated with unintended pregnancies.
Yet, according to the World Health Organization (WHO), an estimated 164 million women worldwide still don’t have access to the contraception they need.
This lack of access has wide-ranging implications, from high rates of unsafe abortions to elevated maternal mortality rates in regions where family planning services are scarce.
Who Has Access to Contraception?
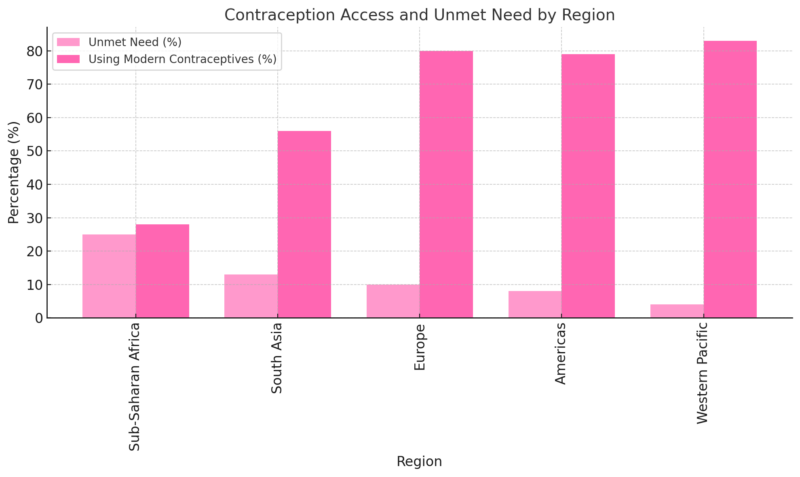
Contraceptive access is not uniformly distributed across regions, with stark differences in usage and availability. Let’s break down some statistics:
- 1.9 billion: The number of women of reproductive age (15-49) globally according to WHO.
- 77.5%: The percentage of women using a modern contraceptive method in 2022 will increase from 67% in 1990.
- 9%: Percentage of women globally who still have unmet contraceptive needs.
- 270 million: Number of women lacking access to modern family planning methods.
These numbers reveal that while Europe and the Americas have high contraceptive use rates, regions like Sub-Saharan Africa continue to struggle with unmet needs, making women more vulnerable to unintended pregnancies and associated health risks.
Contraceptive Prevalence Rates by Region and Continent
Region/Continent
Contraceptive Prevalence (Any Method)
North America
75%+
South America
75%+
Europe
60-74% (Western & Northern Europe)
45-59% (Eastern Europe)
Africa
0-14% (Central Africa)
15-29% (Sub-Saharan Africa)
30-44% (Northern Africa)
Asia
60-74% (East Asia)
45-59% (South Asia)
15-29% (Southeast Asia)
Oceania
45-59%
Middle East
30-44%
- North and South America have some of the highest contraceptive prevalence rates globally, with both continents seeing rates above 75% according to Statista.
- Europe shows a variation, with Western and Northern Europe achieving higher rates (60-74%), while Eastern Europe has slightly lower rates (45-59%).
- Africa has the widest range, with Central Africa showing the lowest prevalence (0-14%), Sub-Saharan Africa with moderate rates (15-29%), and Northern Africa around 30-44%.
- Asia is diverse, with East Asia showing higher rates (60-74%), South Asia at 45-59%, and Southeast Asia lower at 15-29%.
- Oceania generally falls within the 45-59% range.
- The Middle East generally has a contraceptive prevalence rate in the 30-44% range.
Socio-Economic and Geographic Barriers
View this post on Instagram
Women in underprivileged communities, particularly those in rural areas or informal settlements, often lack nearby health centers or family planning services.
For many, the cost of contraception is prohibitive, meaning low-income women disproportionately experience high rates of unintended pregnancies.
In low- and middle-income countries, nearly 74 million women become pregnant accidentally every year.
This situation contributes to 25 million unsafe abortions and 39,000 maternal deaths annually, according to WHO data.
The disparities become even more apparent when looking at specific countries:
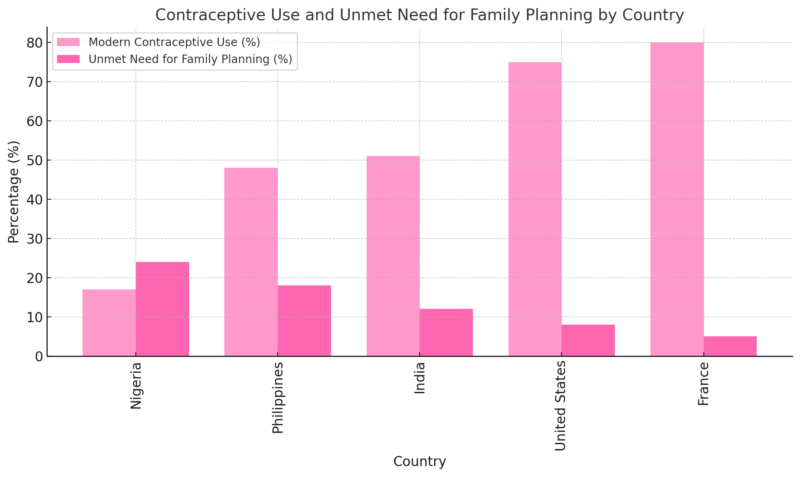
While a country like France has a high usage rate and low unmet needs, Nigeria and the Philippines face significant barriers that limit women’s choices and their ability to make informed reproductive decisions.
Social, Cultural, and Religious Influences on Contraceptive Use
Cultural beliefs, religious teachings, and social expectations are powerful factors in many countries.
In some regions, contraceptive use remains a taboo subject, with women avoiding family planning centers for fear of stigma.
In conservative communities, societal expectations may prevent unmarried women from seeking contraception, and husbands often have considerable influence over family planning decisions.
According to surveys across 34 countries, 14% of married women not using contraception cited their husband’s preference as the main reason.
In countries where men who accompany their wives to family planning centers are viewed as “dominated,” social norms further discourage open family planning discussions within relationships.
The Impact of COVID-19
Many family planning centers were forced to close, and even where services remained open, travel restrictions and economic hardships made access more difficult.
In regions already struggling with healthcare access, the pandemic worsened the situation.
Reports highlight that in countries like Sub-Saharan Africa and South Asia, the impact was severe, leading to even higher unmet needs and an increase in unintended pregnancies.
This underscored the importance of resilient healthcare systems that can maintain essential services during crises.
Misconceptions and Fears
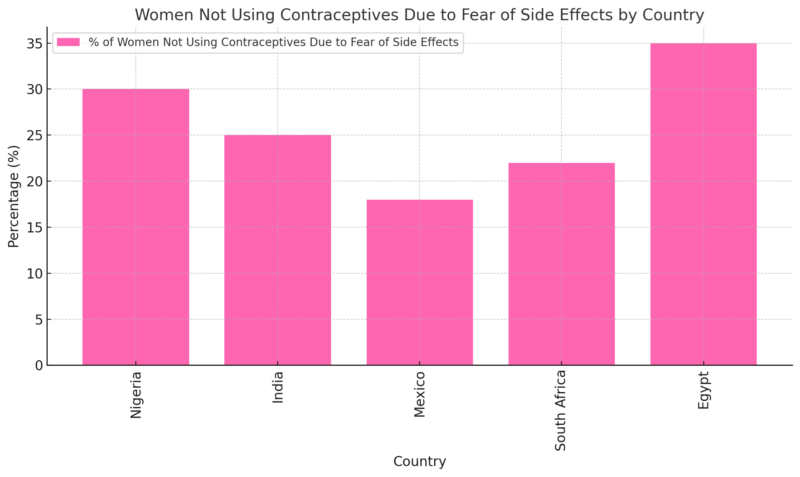
According to WHO studies, two-thirds of sexually active women who wish to delay or limit pregnancies have stopped using contraception due to concerns about health risks.
In a survey by the Guttmacher Institute, 25% of women across 52 countries reported they don’t use contraception because of fears of infertility, depression, or other side effects.
These statistics highlight the need for accessible and reliable information about contraception to help dispel myths and empower women to make informed decisions.
Toward Universal Access to Contraception
The path to universal contraceptive access requires overcoming socio-economic, cultural, and educational barriers.
Governments, non-governmental organizations, and international bodies are working toward this goal, but progress remains uneven.
Addressing the root causes of these gaps, particularly in developing regions, will be crucial in the coming years.
Here are some steps needed to bridge these gaps:
- Expand Access to Family Planning Services: Particularly in low-income and rural areas, more health centers and affordable contraceptive options are essential.
- Educate Communities: Dispelling myths about contraception and promoting awareness can help reduce fear and stigma.
- Engage Men and Community Leaders: Encouraging male involvement in family planning and working with local leaders to shift cultural norms can lead to more supportive environments for contraceptive use.
Final Thoughts
#DYK worldwide, 164 million women lack access to safe & effective contraception when they need it?
Sexual and reproductive health services are essential healthcare for everyone.
They help women and girls:
👧🏻Stay in school
👧🏼Prevent unintended pregnancies
👧🏿Plan their futures… pic.twitter.com/5irXaLL8Wj— World Health Organization (WHO) (@WHO) March 8, 2024
While strides have been made in improving access to contraception, millions of women worldwide still face barriers that prevent them from exercising their reproductive rights.
Ensuring that all women, regardless of location, income, or social standing, have access to contraceptives is not just a health issue—it’s a fundamental human right.
The global community must continue to prioritize family planning services, especially as we work toward achieving gender equality by 2030.
With the rise of women’s health apps, women now have more tools than ever to track their health and make informed decisions about contraception.
By understanding the data and breaking down these barriers, we can create a world where every woman has the freedom to make choices about her own body and future.